Calculator that adds up risk of prostate cancer: Oxford researchers say online tool can help GPs prioritise high-risk patients
- Researchers at Oxford University say their online tool can help GPs
- It is designed to tell men their personal risk of developing prostate cancer
- It is more accurate than the existing prostate specific antigen (PSA) test
A calculator that tells men their personal risk of developing prostate cancer could save thousands of lives.
Researchers at Oxford University say their online tool can help GPs prioritise high-risk patients for scans while reassuring others.
It is designed for use in men with no symptoms and is expected to lead to more tumours being diagnosed early when they are easier to treat.
The calculator estimates an individual’s risk of prostate cancer, aggressive tumours and dying from the disease over the next decade.
It is more accurate than the existing prostate specific antigen (PSA) test routinely used to look for biomarkers in the blood.
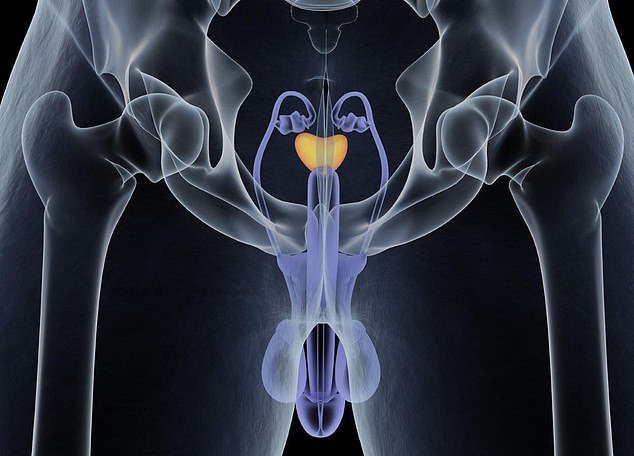
Researchers at Oxford University say their online tool can help GPs prioritise high-risk patients for scans while reassuring others (file image)
The formula combines the PSA result with factors such as age, ethnicity, body mass index, social deprivation and family history. Professor Julia Hippisley-Cox used data of 1.45million men in the UK collected over 20 years to develop the calculator.
She used part of the group to form the equation and tested its accuracy on the others.
The calculator found 68.2 per cent of prostate cancer cases, compared with just 43.9 per cent when using the PSA test.
It was more accurate at detecting high-grade tumours, at 49.2 per cent versus 40.3 per cent, and 67 per cent of deaths against 31.5 per cent.
Professor Hippisley-Cox said: ‘The decision in most primary care practices to refer men who are asymptomatic is based on binary PSA thresholds, although this can lead to too many false-negative and false-positive results.

The calculator found 68.2 per cent of prostate cancer cases, compared with just 43.9 per cent when using the PSA test (file image)
‘Furthermore, a binary threshold does not give any indication for the patient as to their absolute risk of developing prostate cancer and/or clinically significant disease requiring immediate intervention.’
She added: ‘The results show that the risk equation provides a valid measure of absolute risk and is more efficient at identifying incident cases of prostate cancer, high-grade cancers and prostate cancer deaths than an approach based on a PSA threshold.
‘The intended use is to provide a better evidence base for the GP and patient to improve decision-making regarding the most appropriate action, for example, reassurance, repetition of PSA test, referral for MRI, regular monitoring, referral to a urologist, or use of preventative interventions should any become available.’
Professor Hippisley-Cox added: ‘Further research is needed to assess how best to implement the algorithm, and evaluate cost-effectiveness and the impact on prostate cancer diagnosis and subsequent survival.’
Each year in the UK around 48,500 men are diagnosed with prostate cancer and there are 11,900 deaths.
Simon Grieveson, of Prostate Cancer UK, said: ‘Too many men are being diagnosed with advanced prostate cancer.
‘While this research suggests this new model could potentially find more cancers than the PSA test alone, this now needs to be tested in large-scale clinical trials… to determine whether this model could offer real clinical benefit.’ The findings have been published in the British Journal of General Practice.