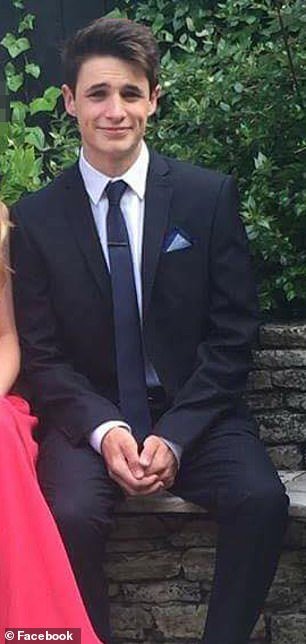
Toby Hudson, 19, was initially unable to speak to a doctor in Weymouth, Dorset due to a faulty phone system and eventually gave up and decided to try again the next day
A university student died from sepsis after trying 50 times to get through to a GP surgery before being wrongly diagnosed with tonsillitis, an inquest heard.
Toby Hudson, 19, was initially unable to speak to a doctor in Weymouth, Dorset due to a faulty phone system and eventually gave up and decided to try again the next day.
When he did get through to a receptionist, Mr Hudson was told he could not have an appointment for at least 48 hours as he was registered at another surgery in Southampton, Hampshire.
Mr Hudson instead decided to go to an urgent care walk-in centre, where he was wrongly diagnosed with tonsillitis and given a course of antibiotics.
His condition deteriorated rapidly over the next 24 hours, and his parents eventually called for emergency services when he became unconscious.
The teenager went into cardiac arrest in the ambulance, but was delayed in getting to Dorset County Hospital because a secondary team of paramedics initially attended the wrong address.
Mr Hudson died on July 4, 2019, two days after he first sought help at the Wyke Regis and Lanehouse Medical Practice.
A post mortem found he died from multiple organ failure due to sepsis which stemmed from infectious glandular fever.
An inquest into his death in Bournemouth heard Mr Hudson had previously been a patient at the Weymouth practice.
He then moved to Southampton to study chemistry and registered at a new clinic close to the campus.
Mr Hudson had been suffering from a cough for around two months before he returned to his family home in Weymouth in the summer of 2019.
He had swollen glands, ‘puffy’ tonsils and a sore throat when his parents told him to speak to a GP.
Giving evidence, Dr Matthew Brook, a partner at the Wake Regis and Lanehouse Medical Practice, admitted issues with the phone system due to a high patient load.
Dr Brook said: ‘We were having tremendous problems with our phone system which could not handle a much higher number of calls.
‘We had updated the system but it was not working correctly. There was a queuing system but in a lot of cases people were waiting a long time and then hanging up.
‘We have had a review since then and nobody recalled taking the call from Toby.’

Mr Hudson died on July 4, 2019, two days after he first sought help at the Wyke Regis and Lanehouse Medical Practice in Weymouth, Dorset
Dr Brook insisted that the correct procedures had been followed.
According to national guidelines, temporary residents should only be seen by a GP if they do not require urgent care.
He said: ‘With temporary residents, receptionists are told to ask whether a patient needs an urgent appointment, within 48 hours.
‘If they do require one within 48 hours we refer them to the urgent care unit.
‘If not, the patient is re-registered and we are then able to make an appointment.’
Nurse practitioner Briony Jefferis said she was ‘not remotely worried’ about Mr Hudson’s symptoms when she examined him at the urgent care centre in Weymouth Community Hospital.
She said: ‘I met with Toby on July 3. He was seen by a triage nurse and then by myself around ten minutes later.
‘He had a normal temperature of 36.1 degrees, a heart rate of 102bpm and rated his pain at an eight out of ten.
‘He did not show any signs of sepsis and his symptoms were consistent with those of tonsillitis.
‘He was given penicillin and told to return if he did not feel an improvement over the next two days. Neither myself nor the triage nurse were remotely worried.’
Mr Hudson’s father, Peter, described the day of his son’s death on July 4.
The father explained how the teenager was taken from his home to Dorset County Hospital in Dorchester, but on the way went into cardiac arrest in the ambulance.
A second crew had to be called, but they initially went to the family’s home address rather than where the ambulance was stopped. It was almost 15 minutes before they arrived at the correct scene.
Mr Hudson was later taken into theatre at the hospital but died later that night.
His father said: ‘I felt there was no urgency. I had to press for action to be taken and for our concerns to be heard.
‘There were issues with communication. The backup crew went to our home address and at from what neighbours have told me they had trouble finding the house.
‘They were knocking on doors before they realised what had happened.
‘They then had to travel almost three miles to where the ambulance actually was through Weymouth summer traffic and through roadworks.
‘We have a lot of concerns about his care.’
The inquest continues.